Cure, Google Gemini
Overview
Experts outline how to assess fit, protect data quality, and decide where decentralization belongs in your clinical trial strategy.
Once considered a niche idea, decentralized trials have become an increasingly accepted option in clinical research, driven largely by advances in digital health technologies. These trials offer greater patient access, faster enrollment, and more flexible study designs. Yet despite this growth and acceptance, decentralized trials are not right for every biotech or healthcare company.
Research teams still need to consider whether a decentralized model truly fits a given study and whether it will produce accurate, useful data. In practice, factors such as therapeutic area, endpoint type, patient population, risk profile, and regulatory expectations all shape how much decentralization is appropriate.
For example, a highly complex interventional trial that demands frequent safety assessments may be better suited to a hybrid approach. An observational or low-risk study, by contrast, may fit a more decentralized model. Understanding those needs early can help teams avoid costly redesigns later, said Dominique Demolle, PhD, CEO and co-founder of Cognivia, a company that works with pharmaceutical and biotech companies to support clinical trials.
“Decentralized trials are diverse and exist on a spectrum,” Demolle said. “At one end, there are traditional, site-based trials with a few added conveniences. At the other end, there are highly distributed models, and most real trials fall somewhere in the middle. While fully decentralized sounds appealing in theory, hybrid models are generally more practical and safer in terms of data management.”
Below, clinical trials experts explore how to think about decentralization without compromising data quality. They outline when decentralized approaches make sense, how to assess fit, and where teams most often run into trouble.
What to Expect From Decentralized Trials
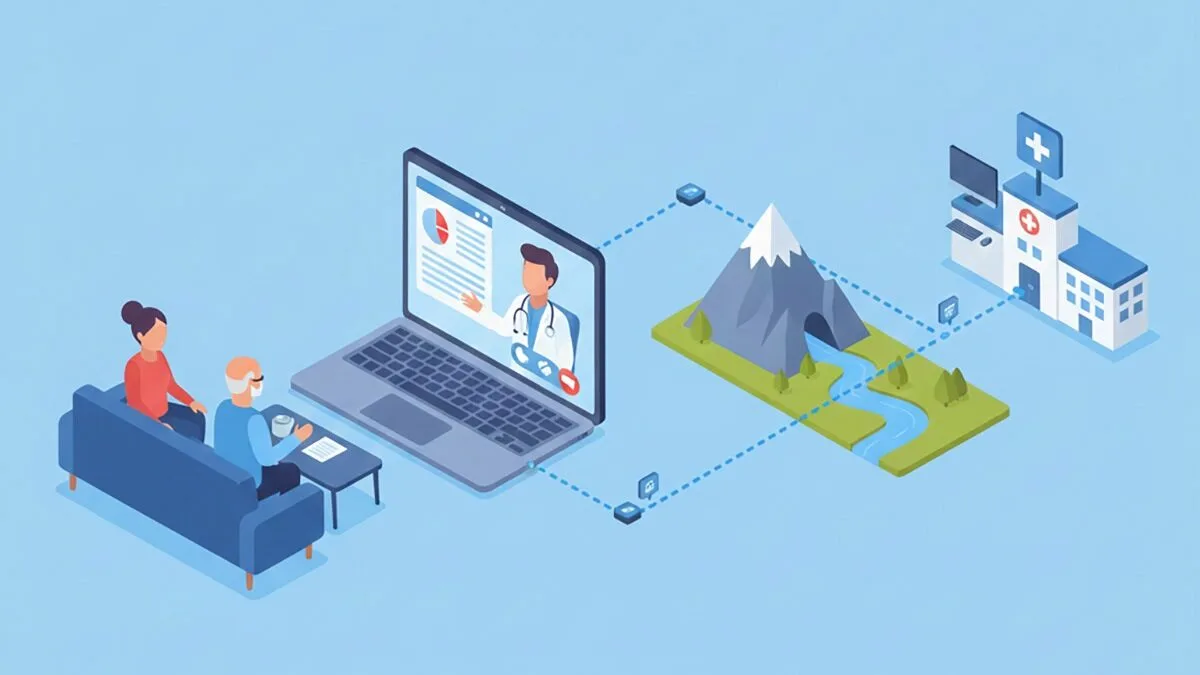
In a decentralized trial, study activities no longer rely on a single physical location. Instead, activities are distributed across digital platforms, home-based options, and local care providers.
That shift can make studies more convenient and accessible for participants. It also changes how communication, oversight, and execution work across a trial. Accommodating those differences often requires tighter coordination across technology platforms, data systems, and mobile health providers.
“Fully decentralized models allow patients to participate without visiting a traditional site, such as a doctor’s office, and take full advantage of remote monitoring through wearables, telemedicine for virtual consultations and assessments, home health visits for check-ups and blood draws, local imaging centers for scans when needed, and direct-to-patient shipment of medications,” said Edward S. Kim, MD, vice physician-in-chief for the City of Hope National Medical Center and system director for City of Hope’s national clinical trials model.
In these settings, trials may use eConsent platforms for secure remote enrollment and electronic patient-reported outcomes for ongoing feedback, he said. Hybrid models blend these remote capabilities with components that still require in-person visits, specialized equipment, or onsite oversight, such as complex procedures or certain safety assessments.
“The key point is that supervision doesn’t disappear in any of these scenarios,” Dr. Kim said. “It shifts by team member and location. Instead of all supervision happening at a physical site, responsibilities are spread across activities. For example, a nurse visiting a patient’s home may report directly into the trial system, and telemedicine visits may include compliance checks that previously occurred in person. This redistribution ensures the same level of safety and data integrity, just through different channels.”
Signs Your Study Design, Endpoints, and Patient Population Fit a Decentralized Approach
Not every clinical study is well suited for a decentralized model. Assessing fit early is critical, particularly because characteristics such as endpoints and patient population can determine whether decentralization strengthens or undermines a study.
Typically, trials with simple procedures, lower risk profiles, and endpoints that can be reliably captured outside a traditional site environment are easier to decentralize. Patients may benefit most when they are geographically dispersed, have limited mobility, and are comfortable using digital tools, said Dr. Kim.
“This makes patients with acute illnesses, cognitive impairments, or those needing close monitoring less suited for remote participation,” he said. “In cancer research, eligibility often depends on treatment phase and stability. Patients on oral therapies or in follow-up care are often better candidates than those undergoing intensive, in-person treatments like chemotherapy.”
For trials involving drug administration, oral medications or self-administered therapies are generally well suited to decentralized models because they can be shipped directly to patients. Treatments that require in-person administration, such as monitored intravenous infusions, still require site visits.
When trials involve devices or digital tools, Demolle recommended starting with the data rather than the technology itself. If an endpoint is objective, clearly defined, and measured consistently, decentralization can work effectively. If an endpoint is subjective, moving it further from a controlled onsite environment introduces more noise.
“Cost and patient convenience are important, but if decentralization harms data quality, it isn’t worth it,” she said. “Garbage in, garbage out.”
How to Decide Which Visits Can Safely Move Remote
When designing a decentralized trial, one of the most important decisions is determining which study visits can safely move to a remote or virtual format. Each visit should be evaluated based on its purpose, the level of clinical oversight required, and its impact on patient safety and data reliability.
Jeffrey Zonder, MD, a hematologist and multiple myeloma specialist who conducted Karmanos Cancer Institute’s first decentralized clinical trial in 2024, suggested starting with the study calendar and breaking each visit into task-level components.
“Tasks such as patient-reported outcomes or digitally collected vital signs are ideal,” Dr. Zonder said. “Other considerations include whether a task carries high risk, or whether an error would compromise the integrity of the entire trial.”
Ultimately, compatibility depends on what a trial is measuring and who the participants are, said Anita Phung, MBBS, a research physician at Lindus Health. “Decentralized approaches work best for oral medication trials with questionnaire-based assessments or long-term follow-up studies where measurements can be captured remotely.”
Patients’ access to reliable internet, comfort with digital tools, and stability of their home environments also matter, she said. Regulatory expectations, protocol complexity, and the need for specialized equipment or trained personnel all factor into these decisions.
How to Protect Data Quality When Patients Collect Measurements at Home
Data quality is often the top concern when considering decentralized trials, particularly as data sources multiply and move outside controlled environments. For decentralization to work, high-quality data must be built into the study design through clear monitoring strategies and defined accountability.
When patients collect measurements at home, data quality becomes both a primary concern and a shared responsibility. Unlike site-based assessments, home data collection introduces variability tied to equipment, environment, and participant behavior.
“The key is to use reliable, validated devices, such as FDA-cleared blood pressure cuffs or wearables, that automatically transmit data to the trial’s electronic system with timestamps,” Dr. Kim said. “This reduces errors from manual entry or missed reporting.”
Patient education is equally important, he said, including simple training videos, hands-on practice, and confirmation that participants understand the process. Built-in alerts for abnormal readings and tracking systems to ensure adherence can further protect data quality. Telehealth visits also offer valuable context by allowing clinicians to see patients in their normal environments.
Demolle emphasized the importance of keeping workflows simple and monitoring data continuously. “The more steps you add, the more drop-off you get.”
She also noted that patient expectations and context change outside the clinic, and those shifts can influence outcomes. “That risk needs to be anticipated and accounted for. In some cases, remote patient-reported outcomes may require re-baselining or covariate adjustment.”
How to Validate Devices, Reduce Variability, and Avoid Protocol Drift
Decentralized trials rely heavily on digital tools and remote assessments, which introduces risks related to device performance, software updates, and user behavior. Addressing those risks early is essential to maintaining data integrity and regulatory confidence.
“The first step is ensuring devices are reliable,” Dr. Kim said. “If we introduce new technology, we test it against trusted standards before the trial begins. Accuracy isn’t a one-time check. We continue monitoring throughout the study.”
Consistency is equally critical. Patients should receive clear instructions and standardized training, often supported by video. Automating data capture reduces manual errors, while regular data reviews, reminders, and check-ins help prevent protocol drift over time.
Dr. Zonder added that validated, standardized devices requiring minimal calibration are preferable. He also flagged the risk that caregivers, including those unknown to investigators, may assist with data collection without adequate training, potentially compromising data quality.
Without strong controls, inconsistencies can accumulate and shift study conduct away from the original protocol. Proactive validation, standardized processes, and ongoing oversight help keep measurements comparable across patients and time points.
Regulatory Considerations to Keep in Mind
Regulators have grown more receptive to decentralized trial models, said Phung, but expectations around safety oversight and documentation remain high. Studies must maintain clear data traceability, comprehensive documentation, and auditable processes across the trial lifecycle.
“Safety monitoring must be proactive, with clear mechanisms for capturing participant-reported side effects and well-defined escalation pathways that meet reporting timelines,” she said. Data security, including encrypted transmission and controlled access, is also essential, along with adherence to applicable privacy regulations.
Dr. Zonder noted that e-consent requires IRB-approved remote processes, including identity verification, confirmation of participant understanding, and delivery of signed consent forms. HIPAA requirements still apply to all remotely collected data, including encryption during transfer and storage. Delegation of authority logs and planned audits remain mandatory.
Regulators ultimately care about patient safety, data integrity, and interpretability, Demolle said. “It’s not enough to show that data were collected remotely. You have to demonstrate that the data can be trusted and meaningfully interpreted.”
How to Choose Vendors, Streamline Technology, and Avoid Over-Engineering the Trial
Technology and vendor choices often determine whether a decentralized trial runs smoothly or becomes unnecessarily complex. It is also easy to over-engineer a study by layering in more platforms than the protocol requires.
Each additional vendor introduces integration, training, and oversight demands. Streamlining technology choices and prioritizing fit-for-purpose solutions can reduce operational burden and data fragmentation.
Demolle advised starting with the scientific question and building the simplest system that supports it. “Avoid stacking tools just because they exist. Each additional component increases friction, risk, and reconciliation challenges. Vendors should reduce burden, not create it.”
Dr. Zonder added that excessive frequency or complexity in remote data collection increases the likelihood of missed or inaccurate data. Over-engineering is a common risk, particularly because decentralized trials are still unfamiliar to many investigators.
When DCTs Increase Cost, Complexity, or Dropout Rather Than Reduce Them
Decentralized trials are often promoted as cost-saving and efficient, but that is not always the case. In some therapeutic areas and patient populations, decentralization can increase expense and operational complexity.
“Costs rise when organizations maintain parallel infrastructures without consolidating,” Dr. Kim said. Vendor sprawl can also drive up fees and management overhead.
Complexity increases when systems do not integrate smoothly, he said, creating additional reconciliation and monitoring work. Dropout risk can rise when patients face digital barriers or when participation feels overwhelming, particularly for those with serious or chronic conditions.
Thoughtful design is critical. Streamlined vendors, integrated systems, and strong patient support can help keep costs flat or lower while preserving data integrity. “If a study cannot be completed reliably,” Dr. Kim said, “the highest cost is unusable results.”
How to Avoid Practical Pitfalls Biotech Founders Encounter
While decentralized trials come with the expectations of speed, scalability, and efficiency, without sufficient operational planning, those expectations can backfire.
Common challenges include unclear ownership across vendors, limited internal resources, and overly ambitious decentralization strategies. Delays, budget overruns, and data quality issues can follow.
“One common miscalculation is assuming that routine smartphone use translates into comfort with clinical trial platforms,” Phung said. She noted that a meaningful share of older adults either lack smartphones or rely on limited data plans.
These challenges can be addressed through intentional design, including dedicated devices with prepaid connectivity, guided reporting tools, and regular participant contact.
Demolle added that assuming perfect internet access or flawless self-reporting is another frequent mistake. Reduced site involvement can weaken data interpretation and safety oversight, and subjective remote data is more sensitive to context.
“Decentralized trials work best when these realities are planned for upfront,” she said, “with simple tasks, strong support, and backup options built in.”








