October 30, 2024
Article
Outside Lander's Office: From DNA Sequencing to AI Insights

Overview
Manolis Kellis, PhD, discusses how artificial intelligence is transforming the very nature of medicine.
Exponential leaps in processing medical information
At the dawn of the genetic sequencing era, the hallway outside of the office of the Whitehead/MIT Center for Genome Research was a busy place.
Eric Lander, PhD, then leader of the Human Genome Project, was racing to be the first to complete and publish his team’s work sequencing human DNA. Among those who frequently crossed paths outside his office were a brilliant graduate student named Manolis Kellis, a science journalist named David Ewing Duncan, and Seema Kumar, who was working at the intersection of scientific research and communications.
Now, two decades later, these three individuals reunited again on stage at the BioFuture conference this week to discuss how artificial intelligence is transforming the very nature of medicine.
The progress since their MIT days is staggering: while the Human Genome Project's first sequence cost $2.7 billion over 10 years, companies like Illumina can now sequence 20,000 complete genomes annually at just $200 each. This dramatic reduction in cost and time has created vast databases of genetic information that, combined with AI, are ushering in the next era of medicine.
"Once you have captured that information, and have big data analyze it, there's no shortage of what you can do to transform healthcare," says Kumar, who is now the CEO of Cure.
The scale of this transformation is difficult to comprehend.
"We've moved from looking at four cells under a microscope to analyzing millions of cells across hundreds of patients simultaneously," said Kellis.
He earned his doctorate in computer science and computational biology, a field he now teaches and innovates as a professor at MIT and member of the Broad Institute. In his own research, AI enables the analysis of 2.4 million cells across 430 patients – a scale of data processing that would be impossible for human researchers alone.
This exponential leap in our ability to process medical information is transforming how doctors diagnose and treat diseases. Traditional medicine relied heavily on physicians observing symptoms and forming hypotheses. Now, AI can analyze thousands of data points simultaneously – from genetic information to medical records to subtle patterns in test results. This data crunching is providing insights that even the most experienced physician might miss.
The impact is already visible in specialties like radiology, where AI systems have demonstrated superior accuracy in detecting certain conditions.
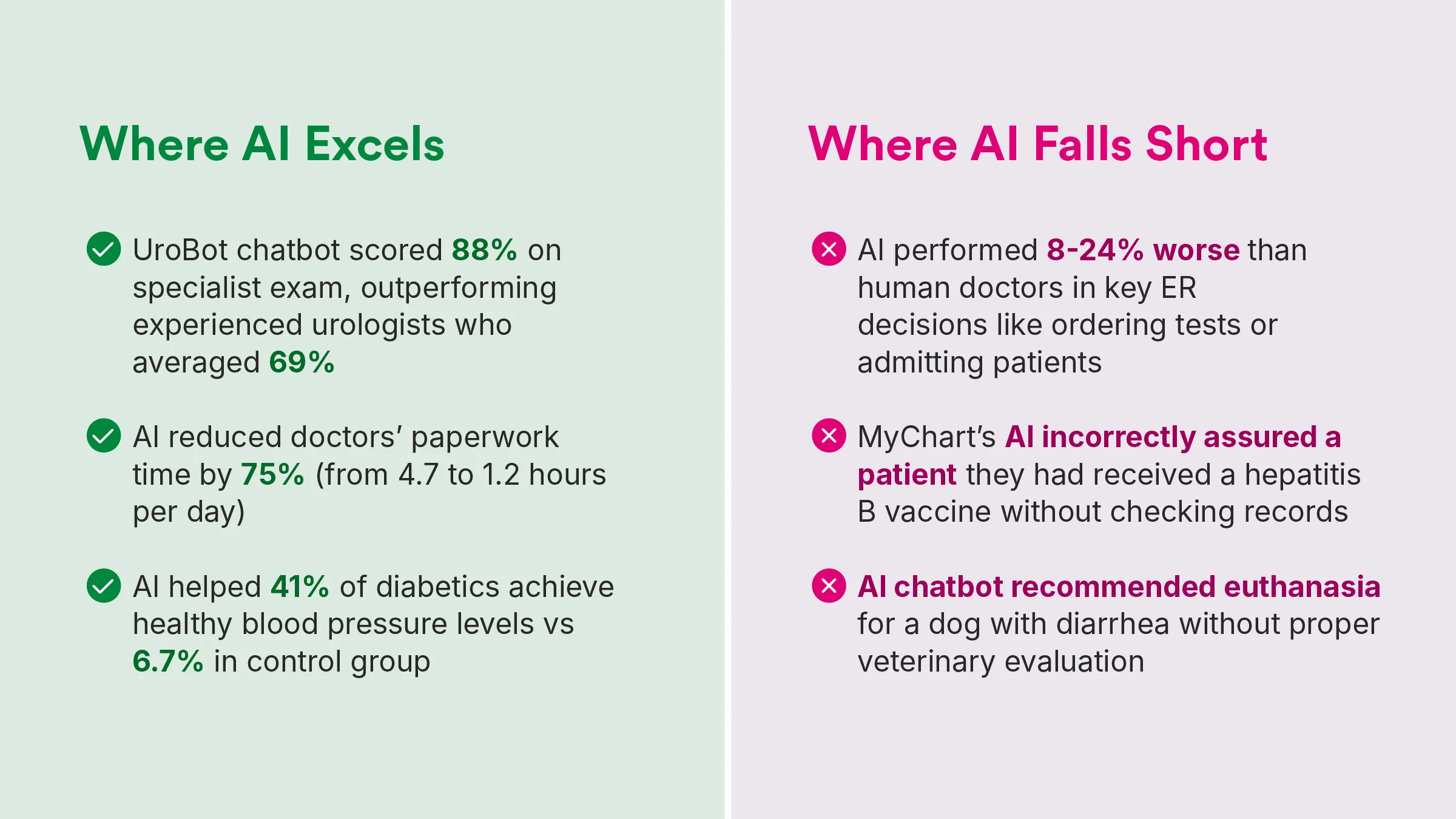
"For very specific tasks, AI has surpassed humans," Kellis said. However, he added that humans are better at “thinking outside the box.” They can understand unusual symptom combinations or rare conditions that don’t fit a common pattern.
This balance between artificial and human intelligence is crucial, especially given healthcare AI's current limitations. Recent headlines have highlighted instances of medical AI making potentially dangerous errors. But Kellis points to a significant advantage of AI in medicine: its ability to learn from mistakes globally.
"When one doctor in Pennsylvania corrects it, another doctor in Nebraska will be able to use that information in their model," he said. "Every doctor improves in isolation, but by having the AI shared across thousands and millions of patients and doctors, we're able to improve continuously."
At Cure, Kumar sees this transformation firsthand. Cure’s Resident Collaboration companies are developing everything from AI-driven drug discovery platforms to smart diagnostic tools. These innovations are already helping doctors summarize patient visits more efficiently, identify potential diagnoses faster, and even predict disease trajectories with greater accuracy. The technology is particularly powerful when dealing with complex diseases.
"Patients are extraordinarily heterogeneous," Kellis said. "We don't just have a monolithic disease that we call diabetes or Alzheimer's."
Recent research has identified multiple distinct subtypes of these diseases, each potentially requiring different treatment approaches. AI helps understand these variations by analyzing patterns across vast patient populations, leading to more personalized treatment strategies.
However, challenges remain. Issues of data sources, data privacy, algorithmic bias, and the need for diverse patient databases must be addressed.
There's also the crucial question of trust, raised by journalist Duncan during the discussion: "How far can it go? Is it going to be correct? When it gets down to it, in our industry, we're talking about human lives."
The answer, according to Kumar, lies in viewing AI not as a replacement for human medical expertise, but as a powerful tool to augment it. "We're not just about innovation for innovation's sake," she says. "Everything we do is focused on one simple goal: cure. Period."
It's a mission that brings full circle the journey that began outside Lander's office two decades ago. Just as the Human Genome Project transformed our understanding of human biology, AI is now transforming how we apply that knowledge to patient care. The doctor of the future will have an AI partner, but it will be the doctor's human insight, empathy, and judgment that turns AI's vast analytical capabilities into better patient outcomes.
"Humans with AI have the ability to integrate so much more data, so many different types of modalities," Kellis said. "And I think that's the opportunity. And then if you are in that healthcare space, this is the place where you can truly, truly make a difference."
Recommended Stories
More about this topic
BioFuture 2024
BioFuture is where today’s leaders convene to transform healthcare as we know it, and the place where tomorrow’s leaders emerge.





